Understanding What Is Andropause in Males: Symptoms and Solutions
Aging brings a host of changes for both men and women. While menopause is widely discussed in women’s health, the male equivalent — andropause — often goes overlooked.
Andropause, sometimes referred to as “male menopause,” involves a gradual decrease in testosterone levels in aging male, leading to various physical, emotional, and psychological symptoms. Unlike the sudden hormonal changes in female menopause, andropause typically occurs gradually, with symptoms that may be subtle but have a lasting impact on men’s well-being.
Understanding male menopause is essential for those experiencing it and their loved ones, as it can profoundly affect one’s quality of life. This article provides a comprehensive overview of andropause, including its symptoms, underlying causes, and potential solutions to manage it effectively.
What is Andropause?
Andropause is a condition characterized by a gradual testosterone levels decline in men, typically starting around the age of 30 and progressing slowly over several decades.
Testosterone, often referred to as the “male hormone,” plays a significant role in regulating libido, energy levels, muscle mass, bone density, and mood stability in men. While women experience a longer phase of hormone reduction during menopause, men experience a more extended, less pronounced decrease in hormone levels. Research shows that testosterone levels generally decrease around the age of 40 in most men, though individual rates of decline vary.
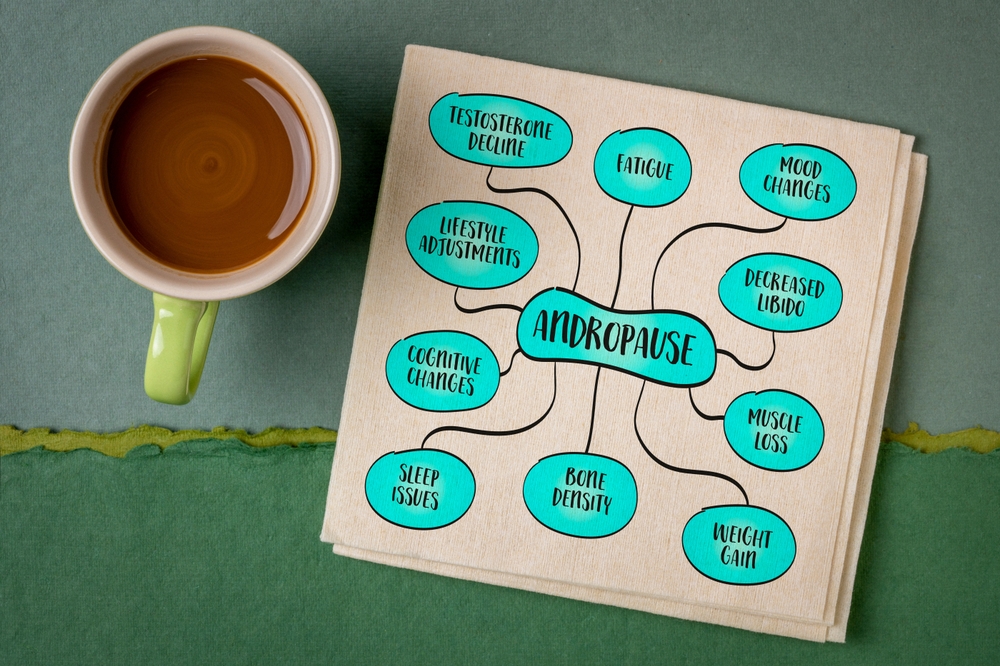
Symptoms of Andropause
The symptoms of andropause – or male menopause – can be wide-ranging, involving physical, mental, and emotional aspects of health. Because they often develop gradually, many men may not initially associate them with andropause.
Let’s look at some of the most common symptoms.
Physical Symptoms
- Decreased Libido and Sexual Dysfunction: Lower testosterone levels can lead to reduced sex drive and erectile dysfunction. These symptoms are among the most prominent and often one of the first signs of male menopause.
- Fatigue and Decreased Energy Levels: Men going through andropause may experience chronic fatigue and a notable drop in energy. Everyday activities can feel exhausting, which can affect both work and leisure pursuits.
- Loss of Muscle Mass and Increase in Body Fat: Testosterone is key to maintaining muscle mass and a lean body composition. As levels decline, men may notice a decrease in muscle strength and an increase in body fat, particularly around the abdomen.
- Bone Density Reduction: Lower testosterone levels can also weaken bones, increasing the risk of osteoporosis. Although more common in women, osteoporosis can affect men with low testosterone, leading to an increased risk of fractures and bone issues.
Psychological and Cognitive Symptoms
- Mood Changes and Irritability: Andropause – or male menopause – can lead to mood swings, irritability, and even depression. Decreased testosterone has been linked to mood regulation issues, making some men feel more easily frustrated or downcast.
- Memory and Concentration Problems: Many men report issues with focus, memory, and cognitive function during male menopause. Research links lower testosterone with reduced brain function.
- Low Motivation and Decreased Self-Esteem: Men with andropause may feel less motivated and experience lower self-esteem. These emotional shifts are often compounded by physical symptoms, which can affect confidence and life satisfaction.
The combination of these symptoms can lead to a decrease in quality of life, which is why understanding andropause is crucial.
Causes and Mechanisms of Andropause
The main cause of andropause – or male menopause – is a decline in testosterone levels, a process that is often influenced by several factors. These include the following.
Aging
Naturally, serum testosterone levels slows as men age. The Leydig cells in the testes, responsible for testosterone production, gradually become less effective over time. Unlike menopause, which occurs over a relatively short timeframe, the hormonal decline in aging male is much more gradual, but the long-term impact can be profound.
Chronic Health Conditions
Obesity, diabetes, and metabolic syndrome can accelerate testosterone decline. These conditions interfere with the body’s hormonal balance and exacerbate symptoms of male menopause. Studies show that men with type 2 diabetes, in particular, are more likely to experience andropause symptoms due to insulin resistance impacting testosterone production.
Lifestyle Factors
Poor diet, lack of exercise, and high levels of stress can also play a role in reducing testosterone levels. Studies show that men with healthier lifestyles tend to maintain higher testosterone levels as they age. Moreover, diets high in processed foods and low in essential nutrients like zinc and magnesium can negatively affect testosterone production.
Genetic Factors
Genetics can influence the rate at which testosterone declines. Some men may experience an earlier onset or a more pronounced drop due to genetic predispositions. Certain genetic markers have been linked to faster declines, and these men may be more prone to experiencing early symptoms of andropause (male menopause).
Hormonal Interactions
Testosterone interacts with other hormones, including cortisol and insulin. High stress can lead to an increase in cortisol, which may, in turn, lower testosterone production. Likewise, insulin resistance in conditions like type 2 diabetes can influence testosterone levels, creating a cycle that perpetuates andropause (male menopause) symptoms.
Environmental Factors
Studies are increasingly focusing on environmental factors, such as exposure to endocrine disruptors found in plastics, pesticides, and certain chemicals. These disruptors can interfere with testosterone levels, and men exposed to high levels may experience earlier or more severe andropause symptoms.
Diagnosis of Andropause
Diagnosing andropause can be challenging due to its gradual onset and the nonspecific nature of symptoms. Many men may attribute their symptoms to general aging or other conditions like erectile dysfunction, delaying proper diagnosis and management. The diagnostic process generally includes the following.
- Medical History and Physical Examination: Doctors will review the patient’s health history and conduct a physical examination, focusing on symptoms like weight gain, fatigue, and decreased muscle mass.
- Laboratory Tests: A testosterone test measures total testosterone, but sometimes, doctors also evaluate free testosterone to gain a clearer understanding.
- Symptom Questionnaires: Tools like the Androgen Deficiency in Aging Males (ADAM) questionnaire can be helpful in identifying symptoms and determining the likelihood of testosterone deficiency.
Accurately diagnosing andropause remains complex due to its overlap with other conditions, such as depression and obesity. A multi-dimensional approach is important, combining patient history, symptoms, and lab tests for an accurate diagnosis.

Treatment Options for Andropause
Effectively managing andropause often requires a comprehensive, multifaceted approach. The following are additional treatment options that may help alleviate symptoms and improve overall quality of life.
1. Advanced Nutritional Therapy
Nutrition plays a significant role in hormonal health, and specific foods and dietary adjustments can support testosterone levels, improve energy levels, and support cognitive function. Dietary strategies include:
- Anti-inflammatory Diet: Chronic inflammation can accelerate the decline in testosterone. An anti-inflammatory diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids (found in foods like salmon, chia seeds, and walnuts) can help reduce inflammation and support hormonal balance.
- Protein-Rich Diet: High-protein foods such as lean meats, eggs, legumes, and tofu help maintain muscle mass, which often diminishes with low testosterone levels. Protein also provides the amino acids necessary for hormone production.
- Healthy Fats: Testosterone is synthesized from cholesterol, so moderate amounts of healthy fats from sources like avocados, olive oil, nuts, and seeds can support testosterone levels.
- Limit Sugar and Refined Carbohydrates: Excess sugar and processed carbs can lead to insulin resistance, which has been linked to low testosterone. Reducing the intake of these foods can support better hormonal health.
2. Mind-Body Techniques and Stress Reduction
Chronic stress is a known contributor to lower testosterone levels, as it elevates cortisol, a hormone that can interfere with testosterone production. Using stress reduction techniques can, therefore, be crucial. Some techniques include:
- Meditation and Mindfulness: Daily meditation can help reduce cortisol levels and improve overall mood. Even short sessions of 10-15 minutes per day have been shown to significantly reduce stress markers.
- Breathing Exercises: Deep breathing techniques, such as diaphragmatic breathing and the 4-7-8 breathing method, can activate the body’s relaxation response, reduce anxiety, and improve sleep quality.
- Progressive Muscle Relaxation (PMR): It involves tensing and then releasing various muscle groups in the body, which can help with stress relief and support mental well-being, especially in men experiencing mood swings or irritability due to andropause.
3. Sleep Quality Improvement
Adequate sleep is essential for maintaining healthy testosterone levels. Studies show that men who get less than 6 hours of sleep per night often experience lower testosterone production. Some strategies to improve sleep include:
- Sleep Hygiene: Avoid screens an hour before bedtime, keep the bedroom cool, and maintain a consistent sleep schedule.
- Natural Sleep Aids: Melatonin supplements, herbal teas (like chamomile and valerian root), and magnesium may aid in achieving deeper, more restorative sleep.
- Cognitive Behavioral Therapy for Insomnia (CBT-I): CBT-I can help address the root causes of insomnia and improve sleep quality, which in turn supports better hormonal health.
4. Peptide Therapy
Peptide therapy is an emerging treatment that utilizes specific chains of amino acids to stimulate the body’s own production of hormones, including testosterone.
Some peptides, like Ipamorelin and CJC-1295, are used to stimulate growth hormone production, which indirectly supports testosterone levels by enhancing muscle mass, reducing fat, and increasing energy. Peptide therapy is typically administered through injections and should be overseen by a healthcare professional.
While research is still ongoing, preliminary studies suggest that certain peptides may offer therapeutic benefits for men experiencing symptoms of andropause.
5. Bioidentical Hormone Replacement Therapy (BHRT)
In addition to traditional testosterone replacement therapy (TRT), bioidentical hormone replacement therapy (BHRT) uses hormones that are chemically identical to those produced by the human body. BHRT may be used to replace testosterone, DHEA, and other androgens that decline with age.
Some people prefer BHRT due to its reputation for being more “natural,” though it’s essential to approach this treatment carefully. Like traditional testosterone therapy, BHRT requires regular monitoring for safety and efficacy, especially since long-term effects are still being studied.
6. Cognitive and Behavioral Therapy (CBT)
The psychological effects of andropause, including mood swings, depression, and anxiety, can sometimes be managed effectively through cognitive and behavioral therapy. CBT focuses on identifying and altering negative thought patterns and behaviors that contribute to emotional distress.
This therapy is particularly helpful for men struggling with motivation, irritability, or self-esteem issues, which are common emotional symptoms of andropause. Working with a therapist, men can develop coping strategies, improve relationships, and enhance their overall mental resilience.
7. Hormone Replacement Therapy (HRT)
One of the most direct treatments for andropause is testosterone replacement therapy (TRT), which involves administering testosterone through injections, patches, gels, or pellets.
Testosterone replacement therapy can improve symptoms such as libido, energy, and mood. However, it also has potential side effects, including an increased risk of cardiovascular issues and prostate health concerns. However, it is important to undergo regular monitoring to ensure safety and efficacy.
Conclusion
Andropause, though less discussed than female menopause, represents a significant shift in men’s lives that can affect physical health, emotional stability, and overall quality of life.
Recognizing the signs, understanding the underlying causes, and taking steps to manage symptoms can empower men to maintain their health and well-being as they age. Combining lifestyle changes, medical interventions, and emotional support can make a substantial difference in the andropause experience.
As awareness grows, more men and healthcare providers are embracing a proactive approach to addressing andropause, ensuring that it becomes a manageable part of aging rather than an inevitable decline.