
What is a 503B Compounding Pharmacy?
In today’s healthcare system, patients require custom medications to address specific health needs not met by mass-produced drugs.
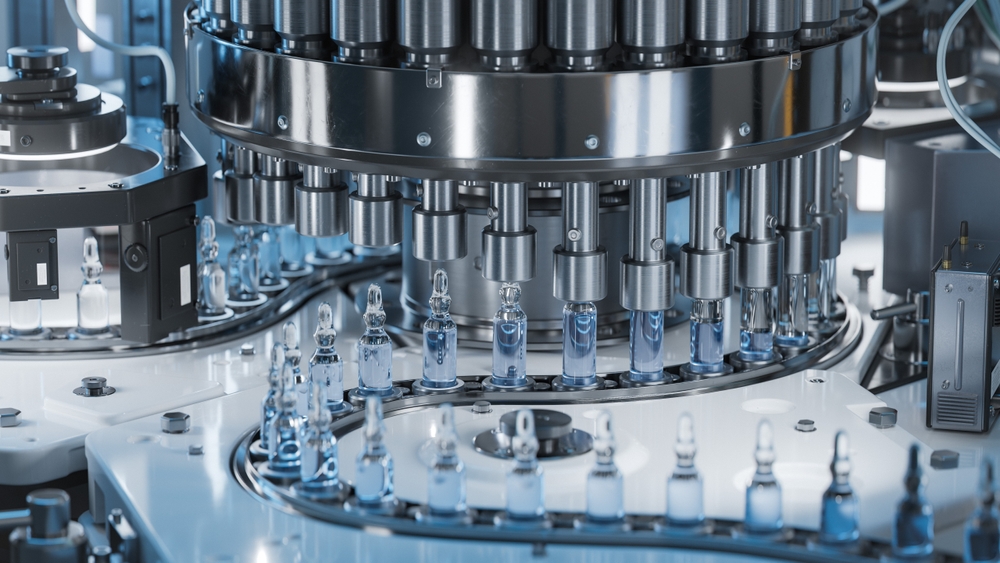
This growing demand has led to the emergence of compounding pharmacies. They create custom medicines to serve patients with unique requirements, whether due to allergies, dosage adjustments, or supply gaps. 503B compounding pharmacies were established to produce large batches of these custom medications while following strict safety and quality standards.
This article explores what sets a 503B compounding pharmacy apart, its role in the drug supply chain, and how it helps healthcare providers find safe, reliable sources for compounded medications.
Introduction to Compounding Pharmacies
Compounding pharmacies play an important role in healthcare by creating custom medications that meet specific patient needs.
A traditional compounding pharmacy, also known as 503A facility, typically operates on a smaller scale, developing medicines for patients based on specific prescriptions. It works closely with healthcare providers to adjust dosages, ingredients, or forms to address patient requirements that commercially available drugs cannot meet.
503B outsourcing facilities operate under strict regulatory standards, allowing them to produce and distribute larger batches of compounded drugs for hospitals, clinics, and other medical settings. While traditional compounding pharmacies serve single patients, outsourcing facilities provide essential medications to healthcare providers, ensuring consistent access to compounded drugs where they’re most needed.
What is a 503B Pharmacy?
A 503B compounding pharmacy, also known as an outsourcing facility, is established to meet the demand for bulk compounded medications without patient prescription, especially for healthcare settings like hospitals and clinics.
Following the Drug Quality and Security Act of 2013, these facilities were created to ensure access to reliable bulk drug substances in large batches, reducing manufacturing costs and providing affordable drugs to consumers.
Unlike traditional 503A compounding pharmacies, which work on a smaller scale and produce medications for individual patients based on specific prescriptions, 503B pharmacies are licensed to produce larger batches for “office use” by healthcare providers. This means that they can supply medicines to be stored and administered as needed without an individual prescription. These medications include:
- Sterile Products: This category includes medications such as injectables like morphine, vancomycin, fentanyl, ophthalmic solutions, and other sterile compounds necessary for patient care in settings such as surgeries, ICU units, or chemotherapy treatments.
- Bulk Drug Substances: 503B pharmacies often compound medications in bulk, which are used to prepare custom formulations with Metformin based on patient-specific requirements, such as testosterone replacement therapies or pain management solutions.
- Critical Care Medications: These include drugs needed for urgent or life-threatening conditions, like anesthetics, antibiotics, and other emergency medications.
- Customized Formulations: Some facilities require medications in specific dosages, concentrations, or delivery methods unavailable commercially, which 503B pharmacies can provide, such as specialized pain creams or compounded hormones.
- Injectables and IV Solutions: 503B pharmacies often produce IV medications, such as electrolytes, vitamins, and other injectable treatments, that may be unavailable from commercial suppliers due to a shortage.
503B outsourcing facilities adhere to strict manufacturing standards, including Current Good Manufacturing Practices (CGMP), which are usually reserved for large-scale pharmaceutical manufacturers.
This ensures that the medicines produced meet rigorous quality and safety standards, providing reassurance to healthcare providers who rely on these drugs to serve their patients effectively. Licensed pharmacists in these facilities oversee the compounding processes and ensure full compliance with regulatory requirements.
The demand for 503B outsourcing facilities is steadily increasing, driven by the healthcare sector’s need for consistent and reliable access to specialized compounded medications. According to Coherent Market Insights, the industry for 503B compounding pharmacies in the U.S. was valued at approximately $920 million in 2021, with projections estimating it could reach nearly $1.5 billion by the end of 2028, growing at a compound annual rate of 7.3%.
This growth reflects the eminent need for bulk compounded medications, especially among hospitals and clinics that depend on 503B facilities to provide safe, high-quality compounded drugs.
Importance of 503B Compounding Pharmacies in the Drug Supply Chain
503B pharmacies emerged from a crucial need for safer, more consistent standards in large-scale compounding.
In 2012, a meningitis outbreak linked to contaminated compounded medications exposed significant safety gaps in compounding practices, leading to tragic health outcomes and a nationwide call for reform. In response, the Drug Quality and Security Act (DQSA) was passed in 2013, establishing 503B compounding pharmacies as a new category with stricter oversight requirements.
These facilities were created specifically to provide healthcare systems with bulk quantities of compounded medications, allowing them to meet demand without compromising quality. In the drug supply chain, these outsourcing facilities help address gaps left by commercial shortages, especially when medications are scarce or high in demand.
By producing large quantities of medicines that adhere to Current Good Manufacturing Practices (CGMP), 503B facilities offer a reliable solution for hospitals and clinics seeking stable, high-grade medicine supplies. This capability is particularly valuable during public health emergencies when the healthcare system faces increased demands that typical manufacturers cannot immediately meet.
Furthermore, 503B facilities allow healthcare providers greater flexibility by ensuring consistent access to compounded medications stored on-site and ready for immediate use. This buffer helps healthcare facilities avoid the disruptions that can occur when relying solely on commercial manufacturers, who may be unable to respond quickly to changes in demand.
Regulatory Standards for 503B Compounding Pharmacies
503B compounding pharmacies operate under rigorous regulatory standards to ensure patient safety and medication quality. Unlike traditional compounding facilities, 503B pharmacies must adhere to federal regulations and FDA oversight, making compliance a central focus of their operations.
One key requirement is meeting current good manufacturing practices (CGMP) designed for large pharmaceutical manufacturers. These standards set clear guidelines on production processes, quality control, and environmental monitoring, helping to prevent contamination and ensure consistent medication quality across batches.
Under the Federal Food, Drug, and Cosmetic Act, 503B, pharmacies must comply with detailed FDA regulations to protect public health. This includes oversight of facility cleanliness, sterile compounding practices, and quality assurance procedures. Compliance with these pharmacy regulations ensures that 503B pharmacies maintain the high standards necessary to produce safe medications on a large scale, providing healthcare providers with a reliable supply of compounded drugs.
Federal food and drug laws require full adherence to safety and quality standards, a commitment that helps build trust among healthcare facilities relying on 503B pharmacies for patient care. The FDA inspects these facilities to ensure they comply with these laws, checking for potential risks and verifying that production processes align with industry best practices.
Moreover, CGMP regulations include specific protocols for handling raw materials, managing inventory, and documenting production steps, all contributing to overall patient safety.

Role of FDA and State Boards in 503B Compounding Pharmacies
The FDA oversees 503B compounding pharmacies, ensuring they follow strict quality and safety regulations.
They conduct routine inspections to ensure these facilities comply with the Drug Quality and Security Act, particularly focusing on Current Good Manufacturing Practices (CGMP). These inspections examine how well a pharmacy maintains sterile environments, controls contamination risks, and consistently produces potent medicines.
This kind of federal oversight prevents safety issues and ensures that compounded drugs meet the needs of healthcare providers and patients.
Local Oversight and Compliance
The pharmacy boards also closely monitor 503B facilities at the state level. They ensure that these pharmacies adhere to local laws, hold the proper licenses, and maintain high standards of care. The state boards monitor the daily operations of these facilities and collaborate with the FDA to address any compliance issues or quality concerns that could impact patient safety.
Collaboration for Patient Safety and Quality Assurance
The combined efforts of the FDA and state boards create a regulatory framework that balances federal and local oversight. This partnership helps protect patient safety and ensures that these outsourcing facilities deliver safe and reliable medications to healthcare providers. By working together, the FDA and state boards strengthen public trust in the quality of compounded drugs.
Current Good Manufacturing Practices (CGMP) in 503B Pharmacies
CGMP ensures quality and safety at 503B compounding pharmacies. These practices guide every step of the production process, ensuring that medications adhere to strict regulations.
CGMP is particularly important for facilities that produce medications on a larger scale because it focuses on maintaining consistency and safety with each batch. For 503B pharmacies, following these standards is mandatory, as they help protect patients and healthcare providers who depend on compounded drugs for required care.
Environmental Monitoring
One of the key elements of CGMP is environmental monitoring. This process makes sure that the pharmacy environment remains sterile and controlled. It involves consistently checking the cleanliness of the air, surfaces, and equipment to prevent contamination. By conducting regular environmental tests, these facilities ensure that every batch they produce is safe, especially when dealing with sterile products.
Quality control
Quality control is another significant factor under CGMP for 503B pharmacies. It involves systematic checks throughout production to ensure that each batch meets the necessary potency, purity, and quality standards.
This includes testing the final products, validating equipment, and overseeing the processes to guarantee that compounded drugs consistently meet established specifications. This quality control process instills confidence in healthcare providers regarding the reliability of the medications they distribute.
Managing Raw Materials
Managing raw materials is also essential under CGMP standards. 503B pharmacies must source active pharmaceutical ingredients and carefully document where each one comes from. They must also test these materials for quality and appropriateness before using them.
Safety and Quality Assurance in 503B Compounding Pharmacies
Safety and quality assurance are central to 503B compounding pharmacies, which produce medications in large batches for healthcare facilities.
These pharmacies follow strict practices to ensure that every compounded drug meets high potency, purity, and patient safety standards. To achieve this, 503B facilities implement a series of rigorous steps:
- Quality assurance begins with sourcing high-quality raw materials, which are carefully tested before use to confirm their purity and suitability.
- Facilities maintain controlled, sterile environments during production to prevent contamination, particularly for drugs requiring sterile compounding.
- When working with bulk drug substances, 503B pharmacies follow specific handling and storage protocols to maintain the integrity of each ingredient.
- After compounding, each batch undergoes thorough testing to confirm consistency, potency, and safety. This includes verifying dosage accuracy and ensuring all compounded drugs meet the required specifications.
By following these structured safety and quality protocols, 503B compounding pharmacies provide healthcare providers with reliable medicine.
Benefits of Using 503B Compounding Pharmacies
Using 503B compounding pharmacies offers several key benefits for both healthcare facilities and patients:
Customized Medication Options
503B pharmacies can produce medications tailored to patients’ specific needs, especially when standard commercial drugs are unavailable or ineffective. This flexibility allows healthcare providers to access medications for specialized treatments.
Consistent Availability for Office Use
Healthcare facilities benefit from a reliable supply of compounded medications, ensuring they can always provide necessary treatments without delays. This is especially valuable for “office use” drugs, allowing immediate access to procedures and patient care.
Cost-Effectiveness
By producing medications in bulk, 503B pharmacies help healthcare providers manage costs more effectively. Large-scale production reduces the cost per unit, making compounded drugs more affordable for facilities and ultimately lowering the cost of patient care.
Scalability
503B facilities are equipped to scale production quickly to meet increasing healthcare demands. Pharmacies can adjust production volumes to ensure healthcare providers have the medicines they need, whether for routine needs or during times of crisis.
Challenges and Limitations of 503B Compounding Pharmacies
503B compounding pharmacies face several challenges and limitations that affect their operations. Some of them are:
High Regulatory Scrutiny
These facilities are rigorously supervised by the FDA and state boards of pharmacy. While this ensures safety and quality, it also leads to frequent inspections and the need for detailed documentation, creating a heavy administrative burden.
Cost of Compliance
Meeting federal and state regulations requires significant investment in training, facility upgrades, and maintaining high operational standards. Adhering to Current Good Manufacturing Practices (CGMP) can be costly, particularly for smaller pharmacies with limited resources.
Complex Manufacturing Processes
Compounding medications involves sophisticated equipment and a skilled workforce, especially in large batches. Ensuring consistency and maintaining quality across large volumes of compounded drugs, particularly sterile products, adds complexity to the production process.
Conclusion
503B compounding pharmacies support the modern healthcare system by providing large-scale, safe, and reliable compounded medications to meet critical needs.
Their adherence to regulatory standards ensures that patient safety remains a top priority, with processes in place to guarantee each medication’s potency, purity, and consistency. These pharmacies help healthcare providers manage drug shortages, offering reliable alternatives when commercial supplies fall short.
Through their dedication to quality and patient care, 503B pharmacies continue to support the healthcare system, reinforcing the trust that providers and patients place in compounded medications.