Starting At $399.00
Regenics offers a range of vitamin and lipotropic injections that you can administer in the comfort of your own home. Whether your goal is losing weight, addressing nutritional deficiencies found on blood tests, or reversing the aging process….
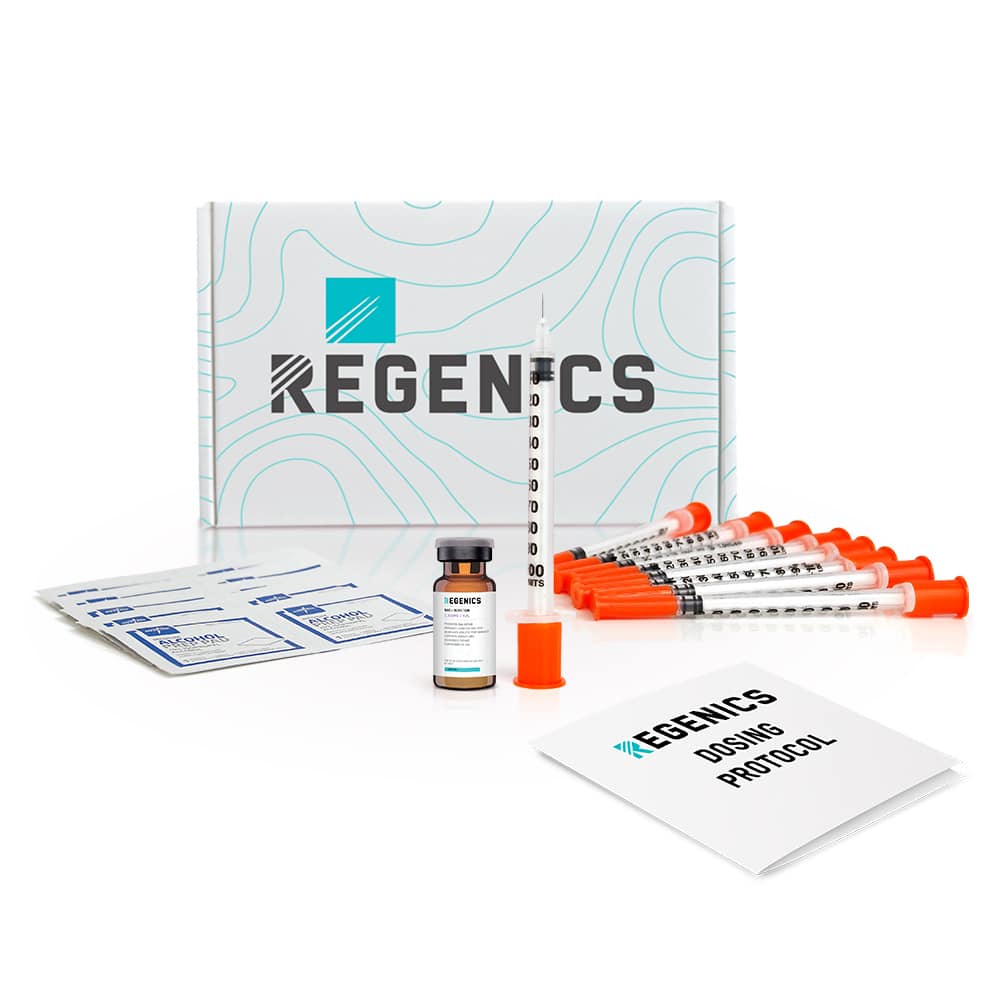
Medication Vial
Injecting syringes
Alcohol wipes
Dosing Instructions
Injecting Instructions
Adjusting this date will cause a lapse in care of your GLP-1 treatment and will require a dose adjustment to keep your care safe and effective.
Canceling your subscription will cause a lapse in care of your GLP-1 treatment and will require a dose adjustment to keep your care safe and effective.